-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Alaa Makke, Raneem Azab* and Jawan Binyassen
Corresponding Author: Raneem Azab, Dental Intern, Dental Teaching Hospital, Oral and Maxillofacial Department, Umm AlQura University, Faculty of Dentistry, Makkah 24225, Saudi Arabia.
Received: March 27, 2024 ; Revised: April 07, 2024 ; Accepted: April 10, 2024 ; Available Online: April 18, 2024
Citation: Makke A, Azab R & Binyassen J. (2024) Correction of Vitamin D Level to Improve Dental Implant Osseointegration: A Case Report. J Oral Health Dent Res, 4(1): 1-4.
Copyrights: ©2024 Makke A, Azab R & Binyassen J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
This case report described the successes of the osseointegration of the dental implant after adjusting vitamin D levels in patients with severely deficient vitamin D levels. The patient lost all of her upper teeth due to aggressive periodontitis. The patient's medical history was reviewed with no significant medical condition. The vitamin D level was corrected to the normal level and four dental implants were placed in the maxilla. Four months later, no early dental implant failure or bone loss was detected.
Keywords: Dental implants, Early dental implant failure, Vitamin D
Abbreviations: EDIF: Early Dental Implant Failure; μg/l: Micrograms per Liter; p. gingivalis: Porphyromonas gingivalis
INTRODUCTION
Vitamin D plays an important role in the maintenance of calcium and phosphate homeostasis within the body. It has a significant role in immune function, physical performance, and bone health [1]. Currently, vitamin D is considered insufficient when the serum level ranges between 21 and 29μg/l, below <20 μg/l as a deficiency, and <10 μg/las a severe deficiency [2-4]. Even though Saudi Arabia is considered a sunny country, there is a high prevalence of hypo vitaminosis D, like other sunny countries in the Gulf region, as a result of decreased skin exposure to sunlight [5]. Vitamin-D deficiency prevalence ranges between 0-97% in the world and is discovered to be at higher levels in regions like the Middle East (Saudi Arabia), and South Asia (Pakistan, 90%) and is highest amongst females [6,7]. While in Europe 2-30% of adults and up to 80% of elderly patients reported with vitamin D deficiency [8]. The known factors for a vitamin D deficiency are insufficient sun exposure, malnutrition, pigmented skin, obesity, premature and dysmature birth, and advanced age [9]. If a patient’s vitamin D level is severely compromised according to the level mentioned in this review, the recommendation is to supplement it with vitamin D to ensure optimal treatment outcomes [10].
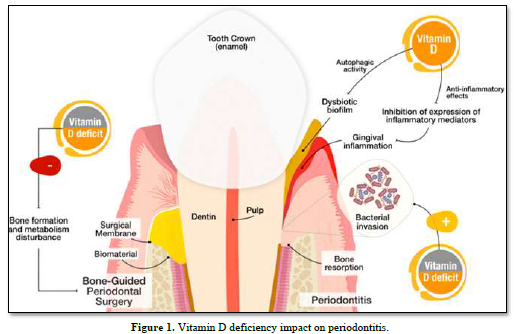
The levels of vitamin D are receiving more attention in oral health [11]. Numerous clinical studies explained the potential reaction of vitamin D to periodontium [11]. There is a significant association between vitamin D deficiency and a high prevalence of gingival inflammation, periodontal destruction, and tooth loss. Increased levels of vitamin D by supplements will result in successful treatment of periodontitis [11-14]. João and colleagues demonstrated in Figure 1 that Vitamin D deficiency impacts periodontitis, in vitamin D deficiency, patients are more susceptible to treatment failure after periodontal regenerative surgery as a result of a disturbance in bone formation and metabolism. In the case of periodontitis, vitamin D may promote p. gingivalis autophagy and anti-inflammatory effect resulting in decreasing gingival inflammation by inhibition of inflammatory mediators’ expression [11].
A correlation between vitamin D on one remodeling and early implant failure has not been proven in humans. Vitamin D promotes bone formation around the implant in rodents [15-19]. Systematic reviews reported that prescribing antibiotics before implant placement significantly reduces early implant infection which may lead to implant failure [20,21]. This article illustrates a healthy young adult patient with vitamin D deficiency and early tooth loss and reveals that implant placement was successful after supplementation of vitamin D.
CASE PRESENTATION
Patient and Surgical Procedures
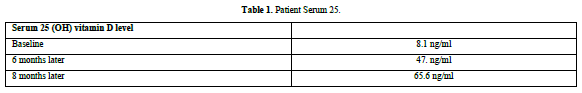
The patient received dental care at Umm Al-Qura Dental Teaching Hospital, Makkah, Saudi Arabia. The patient was medically fit with no systemic disease. The patient had no history of taking regular medication and was negative for nicotine use. The female patient (24 years of age) was not immunosuppressed, irradiated, or received chemotherapy. Verbal and written informed consent were obtained from the patient for the publication of this case report and accompanying images. The patient lost most of her teeth as a result of severe bone resorption and periodontal destruction were the main reasons for extraction. The patient was asked to perform a CBC to check vitamin D levels. The base line vitamin D level showed deficiency (8.1 ng/ml). The patient was advised to start Vita-D 50000 IU Vitamin D once a week for 6-8 weeks. Pt repeated the test 6 months later and the level was 47.8 ng/ml (Table 1). Then, the patient was ready to perform the dental implant surgery.
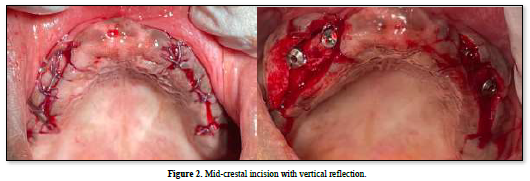
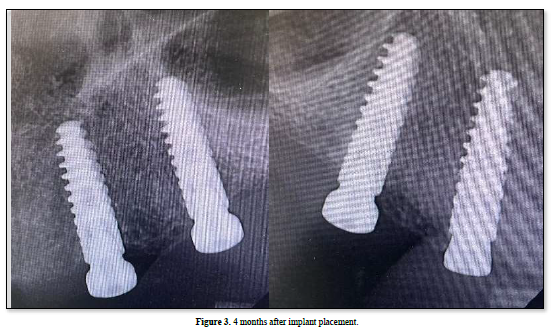
Preoperative orthopantomogram and CBCT were taken in order to evaluate the amount of bone in the ideal position of implant placement. Surgery for implant placement was performed under local anesthesia following a standard operation protocol. A mid-crestal incision in the attached gingiva of the upper edentulous alveolar crest from the canine area of the quadrant until the premolar area on each side with two vertical releasing incisions was performed, after reflecting the mucoperiosteal flap and exposure of the bone, 4 implants were placed in the upper arch by an oral implantologist in order to construct implant-supported maxillary overdenture (Figure 2). Postoperative orthopantomogram after all four implants placement (AnthyogerAxiom®BL PX 3.4 x 12mm), All implants were placed with the same recommended torque of <35 Ncm. Then, healing abutments were placed and the passively mobilized mucosa was closed with resorbablevicryl sutures with a simple interrupted technique. A standard oral antibiotic regimen, mouthwash, and pain killers were applied after implant placement, and post-operative instruction was given. The patient was clinically evaluated after 2 weeks to assess healing. The patient was recalled after 4 months to evaluate implant success to start with the prosthetic superstructure. A periapical radiograph showed full osseointegration with no crystal bone loss (Figure 3). No pain was reported. As well as, no mobility or abnormal pocket depth was noticed.
The successful treatment outcome and the absence of early dental implant failure confirm the recommendations of supplementing with Vitamin D in severely compromised levels. In conclusion, vitamin D seems to be one of the significant factors associated with the osseointegration of dental implants and preventing EDIF.
No Files Found
Share Your Publication :